Ask A Researcher
December 2022
A Look into a Chronic Condition and Pregnancy: Preexisting Diabetes PRAMS Points 2022

The North Dakota Department of Health and the Center for Social Research (CSR) at North Dakota State University (NDSU) continue their collaboration with the North Dakota Pregnancy Risk Assessment Monitoring System (PRAMS), a project that focuses on gathering state-specific data on maternal attitudes and experiences before, during, and shortly after pregnancy to improve the health of mothers and infants. Kendra Erickson-Dockter is a research specialist with the CSR and provides support for projects, such as PRAMS, SOARS, and North Dakota Compass. Kendra received her master’s degree in Sociology at NDSU.
The North Dakota Pregnancy Risk Assessment Monitoring System (PRAMS) is a collaborative surveillance project of the Centers for Disease Control and Prevention (CDC), the North Dakota Department of Health, and the Center for Social Research at North Dakota State University. PRAMS collects state-specific data on maternal attitudes and experiences before, during, and shortly after pregnancy, with the overall goal of reducing infant morbidity and mortality.
To help disseminate study results, a series of analysis documents, PRAMS Points, continue to be released on a variety of topics such as oral health, gestational diabetes,safe sleep, and now, preexisting diabetes.
This article highlights some of the data as displayed in this new Preexisting Diabetes PRAMS Points Dashboard. The dashboard uses data from North Dakota PRAMS gathered from 2017 to 2020 to examine the prevalence of preexisting diabetes and the associated maternal characteristics, outcomes, and health care visit information related to pregnancy. Dashboards such as this, contribute to the ongoing surveillance efforts that can identify populations at risk and help create and evaluate programming and policies to improve health outcomes for pregnant women, babies, and mothers.
Preexisting Diabetes and Pregnancy Background Information
Diabetes is a chronic health condition that impacts how the body’s cells use sugar (glucose) causing blood sugar levels to become too high in the body. Specifically, the body breaks down ingested food into sugar and releases it into the bloodstream. As blood sugar levels increase, the pancreas is signaled to release insulin, a hormone that allows the blood sugar into the body’s cells to be used as energy. If the body does not make enough insulin or if the body cannot use insulin as efficiently as it should, then the blood sugar levels become too high in the body. If this condition is left uncontrolled, a series of health issues can occur, such as kidney disease, heart disease, and vision impairment (1, 2).
The three most common types of diabetes are: type 1, type 2, and gestational diabetes. Type 1 and type 2 diabetes are chronic conditions that a woman has before pregnancy, what we call a preexisting diabetes. Gestational diabetes is a form of diabetes developed during pregnancy.
- Type 1 diabetes occurs when the body does not make insulin. Type 1 diabetes is commonly diagnosed in children or young adults, but people can get it at any age (2, 3).
- Type 2 is the most common type of diabetes. In type 2, the body produces insulin but does not make or use it well. It is most diagnosed in adults but can also be developed at any age (2, 3).
- Gestational diabetes develops during pregnancy in women who do not have preexisting diabetes. Much of the time, gestational diabetes goes away soon after birth (2, 3). See the Gestational Diabetes PRAMS Dashboard for more data and information on this topic.
To increase chances of having a healthy pregnancy and baby, it is important for pregnant women with preexisting diabetes to keep their blood sugar well controlled before and during pregnancy (4). To help prevent associated problems, women with preexisting diabetes can see a health care provider and plan for pregnancy, see a health care provider early and often during the pregnancy, eat healthy foods, exercise regularly, take insulin and medication as directed, quickly control and treat low blood sugar, and monitor blood sugar often (4).
Preexisting Diabetes Data and Trends
On average, in the United States approximately 1 to 2 percent of pregnant women have type 1 or type 2 diabetes. Research has found that preexisting diabetes in pregnant women has increased in recent years. The percentage of pregnant women with type 1 or type 2 diabetes increased 37 percent from 2000 to 2010 (5).
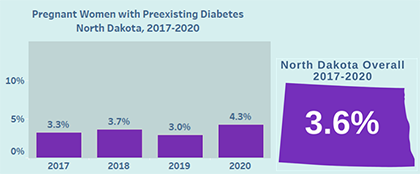
In North Dakota, on average 3.6 percent of pregnant women had preexisting diabetes according to PRAMS data collected from 2017 to 2020. The annual PRAMS preexisting diabetes data vary slightly year to year.
 Preexisting Diabetes by Maternal Characteristics
Preexisting Diabetes by Maternal Characteristics
Maternal characteristics such as body weight, age, education, and race are important to track. They are useful in identifying risk factors and monitoring prevalence and trends, which inform strategies for preventing, controlling, and mitigating risks associated with type 1 and type 2 diabetes before, during, and after pregnancy (1, 6).
When looking specifically at the North Dakota PRAMS data collected from 2017 to 2020, the data essentially follow what literature suggests regarding risk factors and prevalence in terms of maternal characteristics of pregnant women with preexisting diabetes. In North Dakota overall, when comparing against the state’s average of 3.6 percent of pregnant women having preexisting diabetes, the following groups are more likely to have preexisting diabetes while pregnant:
• Those who are obese (Body Mass Index of 30 or higher) (5.3%)
• Those who are American Indian (5.1%)
• Those 30 years and older (4.6%)
• Those with a bachelor’s degree or higher education (4.0%)
• Those with a high school diploma, GED or less education (3.9%)
• Those who had Medicaid as the prenatal care payer (3.8%).
Preexisting Diabetes Associated Outcomes
If not carefully managed, preexisting diabetes can increase the likelihood of experiencing associated outcomes that can negatively impact pregnant women, mothers, and babies. For instance, high blood sugar in women with type 1 or type 2 diabetes around the time of conception increases the babies’ risk of birth defects, miscarriage, and stillbirth. The condition can also lead to an increased risk of pregnant women having high blood pressure (preeclampsia); preterm delivery; a cesarean delivery; babies born with an excessively heavy birth weight, low blood sugar (hypoglycemia), and respiratory distress; and babies developing obesity or type 2 diabetes in the future (2, 5).
When looking specifically at North Dakota PRAMS data collected from 2017 to 2020,
For Pregnant Women who had preexisting diabetes:
• 1 in 15 was diagnosed with high blood pressure during their last pregnancy (6%)
• 1 in 5 had a preterm birth (baby born too early) (19%)
• 1 in 3 had a cesarean delivery (34%).
For Babies who were born to mothers who had preexisting diabetes:
• 1 in 8 babies was born with an excessive birth weight (4,000 grams – 8 pounds 13 ounces – or heavier) (12%).
• 1 in 2 babies stayed in the hospital 3 days or more (34 percent of babies stayed in the hospital 3 to 5 days and 14 percent of babies born to mothers who had preexisting diabetes stayed in the hospital 6 days or longer.
These outcomes are important to track and can inform health care providers and expectant mothers of potential risks. This greater awareness can then lead to approaches to respond to potential complications.
Health care visits before, during, and after pregnancy
One of the best ways of promoting successful outcomes for both baby and mother, is to have a healthy pregnancy and after birth recovery. To improve the chances of having a healthy pregnancy and postpartum care, especially for women with preexisting diabetes, it is important to seek proper health care before pregnancy, and then start and continue regular prenatal and post-pregnancy care with a health care provider to get information, ask questions, and discuss concerns (3, 7).
According to North Dakota PRAMS data collected from 2017 to 2020, two in three women who had preexisting diabetes went to at least one type of health care visit (which could include visits to a nurse, mental care, or dental care) in the 12 months before getting pregnant (68%). Of those women who went to a health care visit:
• 2 in 3 women went to have their teeth cleaned by a dentist or dental hygienist (64%),
• 1 in 2 women went to a regular checkup at the OB/GYN’s office (56%),
• 2 in 5 women went to a regular checkup at the family doctor’s office (44%),
• 1 in 4 women went to a visit for an illness or chronic condition (23%).
During any of those visits, about half of women with preexisting diabetes were talked to about controlling any medical conditions, such as diabetes or high blood pressure (49%) and about one-third of women were talked to about how she could improve her health before pregnancy (35%).
During prenatal visits, about 1 in 2 women with preexisting diabetes who attended these visits were talked to about pregnancy weight gain (53%) and during post-partum visits, approximately 3 in 5 women with preexisting diabetes who attended these visits were talked to about healthy eating, exercise and weight after pregnancy (57%).
Explore the NEW PRAMS Points Preexisting Diabetes and Pregnancy Dashboard to find more data and information on this chronic condition topic!
Note: Overall, please keep in mind that the 2017-2020 North Dakota PRAMS data may not have shown differences in prevalence of preexisting diabetes when comparing among maternal characteristic and associated outcome groups due to a low number of observations. As this chronic condition affects a small proportion of pregnant women, it is sometimes difficult to draw conclusions when taking margins of error into consideration. These data can guide or give an idea what is happening throughout the state, but please use caution when drawing conclusions. As more observations are added each year following this initial dashboard launch, it will be easier to draw comparisons among the group maternal characteristics and associated outcomes associated with this chronic condition.
References
(1) Centers for Disease Control and Prevention. Diabetes Basics: What is Diabetes?. (July 7, 2022). Retrieved October 2022 from https://www.cdc.gov/diabetes/basics/diabetes.html.
(2) March of Dimes. Preexisting Diabetes. (April 2019). Retrieved October 2022 from https://www.marchofdimes.org/find-support/topics/planning-baby/preexisting-diabetes.
(3) Centers for Disease Control and Prevention. During Pregnancy: Diabetes and Pregnancy. (July 14, 2022). Retrieved October 2022 from https://www.cdc.gov/pregnancy/diabetes.html.
(4) Centers for Disease Control and Prevention. During Pregnancy: Type 1 or Type 2 Diabetes and Pregnancy. (July 14, 2022). Retrieved October 2022 from https://www.cdc.gov/pregnancy/diabetes-types.html.
(5) Centers for Disease Control and Prevention. Maternal and Infant Health: Diabetes During Pregnancy. (June 12, 2018). Retrieved October 2022 from https://www.cdc.gov/reproductivehealth/maternalinfanthealth/diabetes-during-pregnancy.htm.
(6) Centers for Disease Control and Prevention. Prevalence and Changes in Preexisting Diabetes and Gestational Diabetes Among Women Who Had a Live Birth — United States, 2012–2016. Retrieved November 2022 from https://www.cdc.gov/mmwr/volumes/67/wr/mm6743a2.htm.
(7) National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development. (January 31, 2017). Retrieved April 2022 from https://www.nichd.nih.gov/health/topics/pregnancy/conditioninfo/prenatal-care.
PRAMS Information
More information about the PRAMS project and PRAMS data can be found at www.health.nd.gov/prams.
Explore the NEW PRAMS Points Preexisting Diabetes Dashboard today!

Other PRAMS POINTS
• Pregnancy and Oral Health (May 2021)
• Gestational Diabetes (July 2022)
• Babies Safe Sleep (August 2022)
